1. Select a discrete app icon.

notes
Your Responses to Trauma Are Normal: How Domestic Violence Can Affect Your Mental Health
Trauma-related mental health conditions like CPTSD, PTSD, depression or anxiety are common in domestic violence survivors
- Sep 14, 2025

When you live with domestic violence, you experience trauma. That trauma can trigger conditions like post-traumatic stress disorder (PTSD), complex post-traumatic stress disorder (CPTSD), depression and anxiety. It’s important to understand that these reactions are normal human responses so you can take steps to access the support and healing you need.
As a domestic violence survivor, watch for signs and symptoms of these trauma-related mental health conditions. Keep in mind that these symptoms can overlap.
Post-Traumatic Stress Disorder (PTSD)
A single or short-term traumatic event can trigger PTSD. Symptoms may include:
- Intrusive thoughts or flashbacks
- Nightmares
- Avoidance of reminders (people, places or conversations)
- Hyperarousal (being jumpy or easily startled)
- Negative beliefs about oneself or the world
- Numbness or detachment
- Insomnia or disrupted sleep
“With PTSD, there are flashbacks to previous events and hypervigilance where you see threats that aren't really threats. It changes the lens from which you see life. After a traumatic event, you see things from the lens of potential threat or injury,” says Lindsey Yochum, LMFT, clinical director at Attune Counseling.
There is some debate among professionals whether PTSD should be classified as a disorder, but rather as a response, and a normal one at that. After all, seldom does someone endure trauma without coming out on the other side with lingering effects.
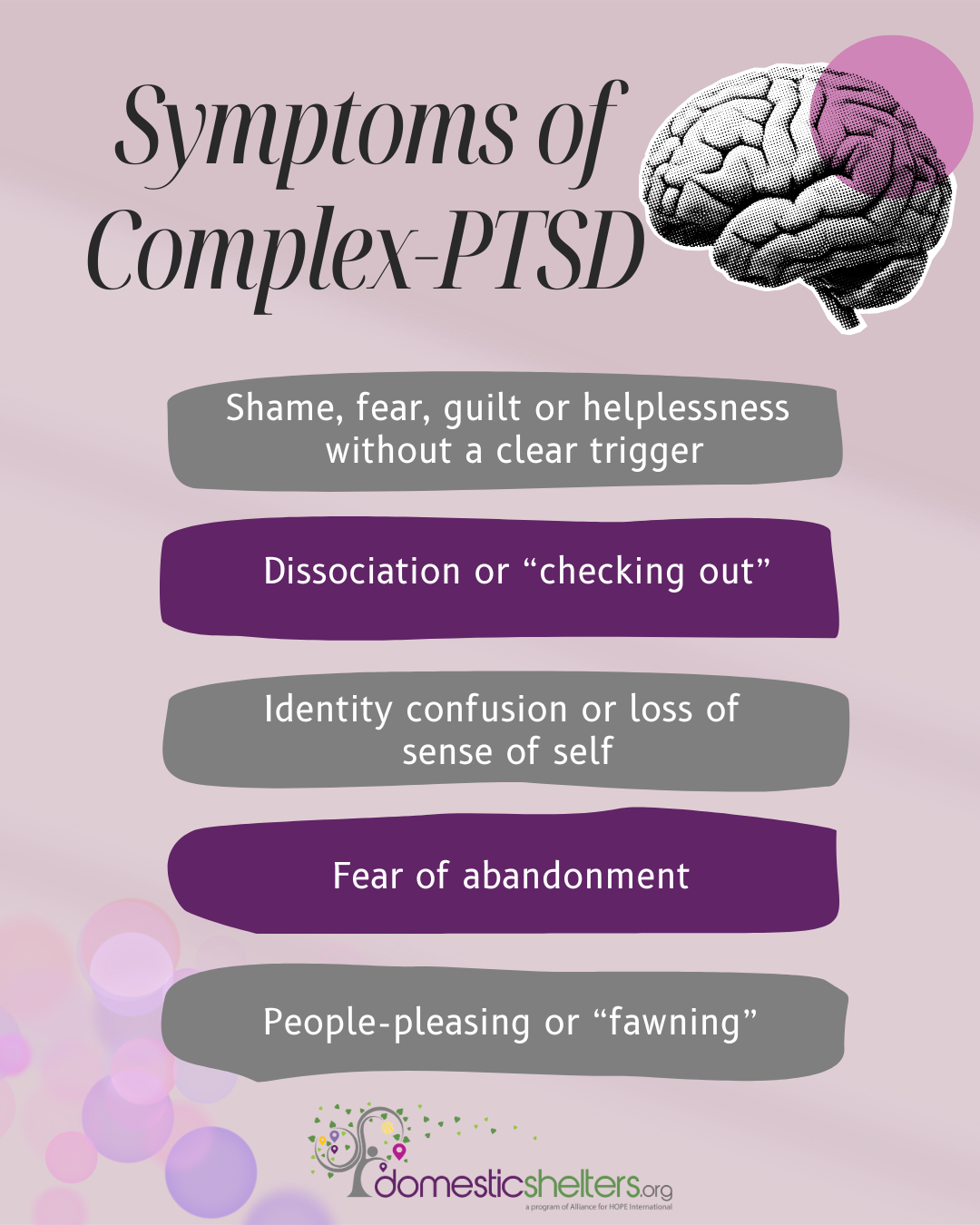
Complex Post-Traumatic Stress Disorder (CPTSD)
CPTSD is related to PTSD, but it stems from repeated trauma rather than a short-term event. “CPTSD is an emotional and physical response to ongoing or long-term threat of harm, danger or neglect,” says Kim Rippy, LPC, a trauma and anxiety specialist at Keystone Therapy Group.
Many domestic violence survivors experience the long-term abuse or coercive control that can lead to CPTSD. Symptoms may include:
- Shame, fear, guilt or helplessness without a clear trigger
- Feeling worthless
- Having trouble trusting others
- Fear of abandonment
- “People-pleasing” or fawning
- Identity confusion or loss of sense of self
- Dissociation or “checking out”
- Relationship difficulties, especially around conflict or intimacy
- Hypervigilance, or always bracing for impact
Depression
“With depression, you are looking at a severe lack of interest, motivation and not feeling like yourself. You feel like you don't have as much hope as you did in the past,” Yochum says. You may notice:
- Persistent sadness or hopelessness
- Loss of interest or pleasure in things you once enjoyed
- Fatigue or low energy
- Changes in sleep or appetite
- Trouble concentrating or making decisions
- Feelings of worthlessness or guilt
- In some cases, thoughts of death or suicide
Anxiety
“Anxiety is a state of emotional and physical hyperarousal in response to a non-immediate trigger or anticipation of danger without danger being actually present,” Rippy said.
Anxiety can include:
- Excessive worry or fear
- Racing thoughts
- Muscle tension
- Irritability or restlessness
- Sleep problems
- Panic attacks
How Common Are These Conditions in Domestic Violence Survivors?
Most domestic violence survivors experience some combination of PTSD, CPTSD, depression and anxiety.
“Up to 84 percent of DV survivors meet criteria for PTSD at some point during or after the abuse. Many report chronic PTSD symptoms, especially when the abuse was ongoing, included coercive control or involved threats to life or safety,” says Nina Batista, LCSW, a trauma specialist in private practice and a DV survivor.
Shari Botwin, LCSW, is a private-practice therapist who specializes in trauma. Her experience supports that statistic. “I have not worked with a client in the last 29 years with a history of intimate partner violence (IPV) who does not struggle with PTSD, depression or anxiety. IPV significantly increases the risk of mental health issues, with PTSD being particularly common among female survivors,” she says.
Psychological abuse is linked with depression and anxiety. Botwin says her clients who have experienced emotional abuse often struggle even more with lack of confidence, hopelessness and difficulty trusting others.
Your Responses to Trauma Are Normal
Batista points out that trauma responses aren’t signs of disorder, they’re signs of survival and normal human responses to danger, betrayal and emotional harm.
And Rippy says, “Almost every diagnosis in the DSM-5-TR [a guide for mental health providers] should be considered a normal human response to someone’s life experiences. The symptoms of PTSD and CPTSD all started as the brain and body's way of coping with ongoing fear or trauma. The sympathetic nervous system is incredibly effective for helping us to survive,” she says.
Trauma therapist Allison Briggs with Being Real agrees. She says, “What we pathologize as mental illness is often the nervous system’s incredibly intelligent attempt to survive the unbearable.” Responses to DV like hypervigilance, avoidance, emotional numbing and even people-pleasing may be ways you show strength and resourcefulness in a hostile environment.
How To Move Toward Acceptance and Healing
Veronica West, a psychologist and founder and lead content creator of My Thriving Mind, recommends reframing trauma symptoms as a mark of survival, not failure. “Let’s retire the idea that mental health symptoms are something to be ashamed of. Anxiety, depression, CPTSD — they’re not character flaws. They’re battle scars, and they mean you survived.”
It can help to treat yourself like you would treat a friend. “The truth is, when you stop being hard on yourself and give yourself the grace, love and compassion you deserve, it makes you more capable of moving forward, connecting with hope and being able to make changes,” Yochum says.
Domestic violence can leave you with deep emotional scars. Even though your responses to the trauma are normal, they are also mental health wounds that need intervention and support. “If symptoms of PTSD, depression or anxiety are preventing people from functioning in their personal or professional lives, psychological support is warranted,” Botwin says.
Trauma-informed therapy can give you a safe space to process abuse, challenge your negative beliefs and learn new ways to cope. She says, “Therapy helps manage trauma symptoms like anxiety, depression, flashbacks and sleep disturbances. Therapists can help survivors reclaim their self-worth, build self-esteem and navigate the journey towards healing and empowerment.”
Rippy says that working with a therapist who specializes in complex trauma is important, because it can help you see that your symptoms were what protected you and helped you survive in the midst of trauma.
As part of your therapy, your provider may recommend techniques such as:
- Eye movement desensitization and reprocessing (EMDR)
- Brainspotting, a technique similar to EMDR and used to help release emotions
- Somatic therapies, which are centered on the body
- Internal family systems (IFS), which helps identify and address your sub-personalities
- Education about how trauma reshapes the nervous system
It can also help to connect with others who understand what you’ve been through. In-person or online support groups can validate your feelings, help you cope and give you hope.
“You need to not only know you are not alone, but feel you are not alone. No one can understand it but the people who have gone through the same thing. To be able to be seen and understood in this experience is huge,” Yochum says.
Hotlines, shelters, advocacy organizations and trusted loved ones can help you connect with the care you need. “Getting help starts with finding safe, trauma-informed support,” says Anat Joseph, LCSW, a psychoanalyst at MyPsychotherapy. “Healing from abuse isn’t about ‘fixing’ yourself — it’s about rebuilding safety, self-trust and a life that belongs to you.”
Keep in mind that there’s no single path to healing, and no right way to respond after trauma. Whether you feel stuck, numb, anxious or angry, your body and mind are doing their best with what they’ve been through. Connect with help when you feel ready so you can begin the healing process.
Donate and change a life
Your support gives hope and help to victims of domestic violence every day.







